In 8-10% of trauma scenarios involving a blunt or penetrating force to the abdomen, consistent with a road traffic collision, fall or violent attack, renal injury will occur (Anelsma de Costa et al., 2016). Considering that the kidneys receive 20% of cardiac output via the renal artery, any compromise to the vessels is serious. Therefore, a rapid, accurate diagnosis of renal injury is vital to promote the best outcome for trauma patients (O’Callaghan, 2009).
According to Sessa et al. (2015), contrast-enhanced multi-detector computed tomography (CT) is the gold standard for the imaging of renal trauma. Not only is CT readily available in the emergency department, but it has the capacity to produce 3D rendering to assess compromised blood vessels (Peng et al., 2016). The study by Peng et al. (2016) did not consider recent developments in imaging modalities, including comparisons of multi-slice CT and intravenous pyelography (IVU). It concluded ultrasonography was a valuable tool, but MSCT was superior with a diagnostic accuracy of 100%. Considering IVUs are now increasingly rare in clinical practice, and multi-detector, rather than multi-slice, CT is more relevant, its validity is questionable. However, its conclusion is supported by other recent UK studies, such as that by Torrance et al (2018). Amerstorfer et al (2015) contends that, considering radiation protection, ultrasound can be reliably used as a first line diagnostic tool, especially for paediatrics. This is reaffirmed by Sessa et al.’s (2015) conclusion that contrast-enhanced ultrasonography (CEUS) is comparable to contrast-enhanced multi-detector computed tomography (CEMDCT) for abdominal trauma imaging. While this study includes liver, spleen and kidney injuries under the umbrella term of abdominal trauma, it is still valuable as in reality, it is important for a modality to provide accurate diagnostic information about injuries in other surrounding organs in one scan. CEMDCT was used a reference modality, making the assumption that it is 100% accurate. CEUS had a sensitivity of 96%, a specificity of 99%, NPV of 98%, PPV of 98% and overall accuracy of 98% compared to CEMDCT. This leads to the conclusion that the use of contrast-enhancement makes ultrasonography comparable in diagnostic accuracy to the more expensive, higher risk examination of CT.
Even with an accurate imaging modality, the renal injury patient pathway is dependent on the severity of injury as classified on the American Association for the Surgery of Trauma (AAST) renal injury scale (1989). While it is useful for categorising a broad range of injuries, several literature sources have drawn attention to the scale’s limitations due to inter-observer variability (Torrance et al., 2018). Pretorius et al. (2018) explain that inter-observer variability is results in different diagnoses based on differences in personal interpretation of scans. This is more pronounced for higher grades of renal injury. The study suggests that some categories need modification to ensure that patients receive the appropriate treatment as soon as possible.
An update on the AAST has been published very recently and focusses on correct identification of vascular damage. For example, vascular thrombosis, segmental renal artery or vein injury and all collecting system injuries are classed as Grade IV injuries, while a devascularized kidney with active bleeding characterises a Grade V injury (Kozar et al., 2018). The revision of the scale includes CT-diagnosed vascular injury as a general term, accounting for the fact that scanners are unable to differentiate between a pseudoaneurysm and an arteriovenous fistula. An arteriovenous fistula is a join between an artery and a vein (Siddiky and Sarwar, 2014). Pseudoaneurysms are caused by deceleration on the artery producing a bleed that is contained by surrounding tissues, resulting in an unstable, potentially fatal lesion (Pastorin et al., 2007). Kozar et al. (2018) support this and explain that delayed imaging is important in assessing renal injury. In CT, contrast that decreases in attenuation is indicative of vascular injury while contrast that increases in size or attenuation evidences active bleeding. This, therefore, reiterates the value of contrast in renal trauma imaging, as well as the potential need for examination by multiple modalities. Dual phase imaging is recommended in the diagnosis of vascular injuries because it allows organ injury to be assessed better than if only one phase is used. Doppler ultrasonography is also able to highlight this injury by demonstrating erratic backwards and forwards flow.
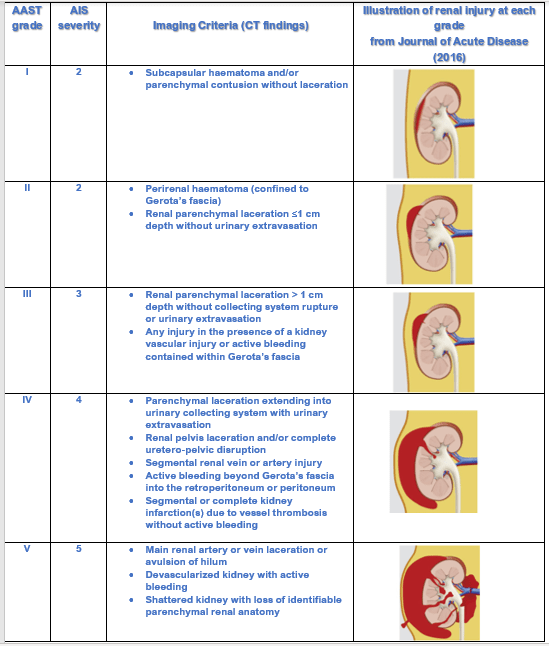
Table: Kidney Injury Scale. Adapted from Journal of Trauma and Acute Care Surgery (2018).
The AAST grading scale highlights that renal trauma can be highly complex, due to the kidneys’ vascularity, emphasising the need for an accurate diagnosis to initiate an appropriate and effective treatment pathway. Various studies demonstrate that contrast-enhancement is important in ruling out vascular injury. CT is recognised as a gold standard in terms of accuracy, availability, assessment of other organ injuries, and post-image rendering. Yet, contrast-enhanced ultrasonography can complement the use of CT due to its ability to provide accurate diagnostic information about vascular injury, its comparative cheapness and lack of radiation dose to the patient.
References:
Amerstorfer, E., Haberlik, A., and Ribbocara, M. (2015) Imaging assessment of renal injuries in children and adolescents: CT or ultrasound? Journal of Pediatric Surgery [online]. 50 (3), pp. 448-455. Available from: https://doi.org/10.1016/j.jpedsurg.2014.07.006 [Accessed 20 October 2018].
Anelsma da Costa, I., Amend, B., Stenzl, A., and Bedke, J. (2016) Contemporary management of acute kidney trauma. Journal of Acute Disease. 5(1), pp. 29-36. Available from: https://doi.org/10.1016/j.joad.2015.08.003 [Accessed 23 October 2018].
Hadjipavlou , M., Grouse, E., Gray, R., Sri, D., Huang, D., Brown, C., and Sharma, D. (2018) Managing penetrating renal trauma: experience from two major trauma centres in the UK. BJU International [online]. 121(6), pp. 928-934. Available from: https://doi.org/10.1111/bju.14165 [Accessed 20 October 2018].
Kozar, R., Crandall, M., Shanmuganathan, K., Zarzaur, B., Coburn, M., Cribari, C., Kaup, K., Schuster, K., and Tominaga, G. (2018) Organ Injury Scaling 2018 Update: Spleen, Liver, and Kidney. Journal of Trauma and Acute Care Surgery [online]. Available from: https://www1.uwe.ac.uk/library [Accessed 23 October 2018].
Moore, E., Shackford, S., Pachter, H., McAninch, J., Browner, B., Champion, H., Flint, L., Gennarelli, T., Malangoni, M., and Ramenofsky, M. (1989) Organ injury scaling: spleen, liver and kidney. Journal of Trauma and Acute Care Surgery. 29(12), pp. 1664-1666.
O’Callaghan, C. (2009) The Renal System at a Glance [online]. Hoboken: Wiley-Blackwell. [Accessed 31 October 2018].
Pastorin, R., Rodriguez, N., Polo, A., Vicente, J., and Lujan, M. (2007) Posttraumatic giant renal pseudoaneurysm. Emergency Radiology [online]. 14(2), pp. 117-121. Available from: https://doi-org.ezproxy.uwe.ac.uk/10.1007/s10140-007-0573-5 [Accessed 23 October 2018].
Peng, N., Wang, X., Zhang, Z., Fu, S., Fan, J., Zhang, Y. (2016) Diagnosis value of multi-slice spiral CT in renal trauma. Journal of X-ray Science and Technology [online]. 24 (5), pp. 649-655. Available from: https://content.iospress.com/articles/journal-of-x-ray-science-and-technology/xst585 [Accessed 20 October 2018].
Pretorius, E., Zarrabi, A., Griffith-Richards, S. Harvey, J., and Ackerman, H. (2018) Inter-rater reliability in the radiological classification of renal injuries. World Journal of Urology [online]. 36(3), pp. 489-496. Available from: https://doi.org/10.1007/s00345-017-2166-6 [Accessed 23 October 2018].
Sessa, B., Trinci, M., Ianniello, S., Menichini, G., Galluzzo, M., and Miele, V. (2015) Blunt abdominal trauma: role of contrast-enhanced ultrasound (CEUS) in the detection and staging of abdominal traumatic lesions compared to US and CE-MDCT. La radiologica medica [online]. 120 (2) pp.180-189. Available from: https://link.springer.com/content/pdf/10.1007%2Fs11547-014-0425-9.pdf Accessed 31 October 2018].
Siddiky, A., and Sarwar, K. (2014) Management of arteriovenous fistulas. BMJ [online]. 349 (7981). Available from: https://www.bmj.com/content/349/bmj.g6262.full [Accessed 31 October 2018].
Torrance, R., Kwok, A., Mathews, Elliot, M., Baird, A., and Lucky, M. (2018) Management of renal injury in a UK major trauma centre. Trauma [online]. 0 (0), pp.1-6. Available from: https://doi.org/10.1177/1460408618802997 [Accessed 22 October 2018].
Hi Rosie,
This is another nice post, this time looking at imaging renal trauma. You have provided some useful analysis of the various options for imaging and there is evidence of evaluation of your sources. “The study by Peng et al. (2016) did not consider recent developments in imaging modalities, including comparisons of multi-slice CT and intravenous pyelography (IVU). ” – I am not sure what you mean here. IVUs have been considered “defunct” for a number of years now, certainly well before Peng et al published, so consideration of them is surely not relevant, especially in an acute trauma situation. “and multi-detector, rather than multi-slice, CT is more relevant, ” – you do realise that the terms MDCT and MSCT are interchangeable and that they mean the same thing? The use of the table is good, but do refer to it in the main body of your text.
Overall, another good piece of work.
Simon
LikeLike